Genital herpes is a sexually transmitted disease (STD) caused by the herpes simplex virus type 1 (HSV-1) or type 2 (HSV-2). This virus attacks healthy cells in your body, hijacking them and forcing them to crank out thousands upon thousands of exact replicas of the Herpes virus, which then move to attack neighboring healthy cells. Not long after becoming infected, the cells work themselves to death, and when enough cells die, it leads to lesions (sores) on the surface of the skin.
It is estimated that one in five persons in the United States has genital herpes; however, as many as 90 percent are unaware that they have the virus.
This is because many people have very mild symptoms that go unrecognized or are mistaken for another condition or no symptoms at all.
Because signs and symptoms can vary a great deal, the only way to know for sure if you have Herpes is to get Tested.
What are the Symptoms of Herpes?
The first symptoms of herpes usually occur within the first two weeks after the virus is transmitted.
Sometimes the symptoms are uncomfortable or even painful, but many times the symptoms are rather mild, hard to notice, and are often mistaken for another skin condition like an insect bite or rash.
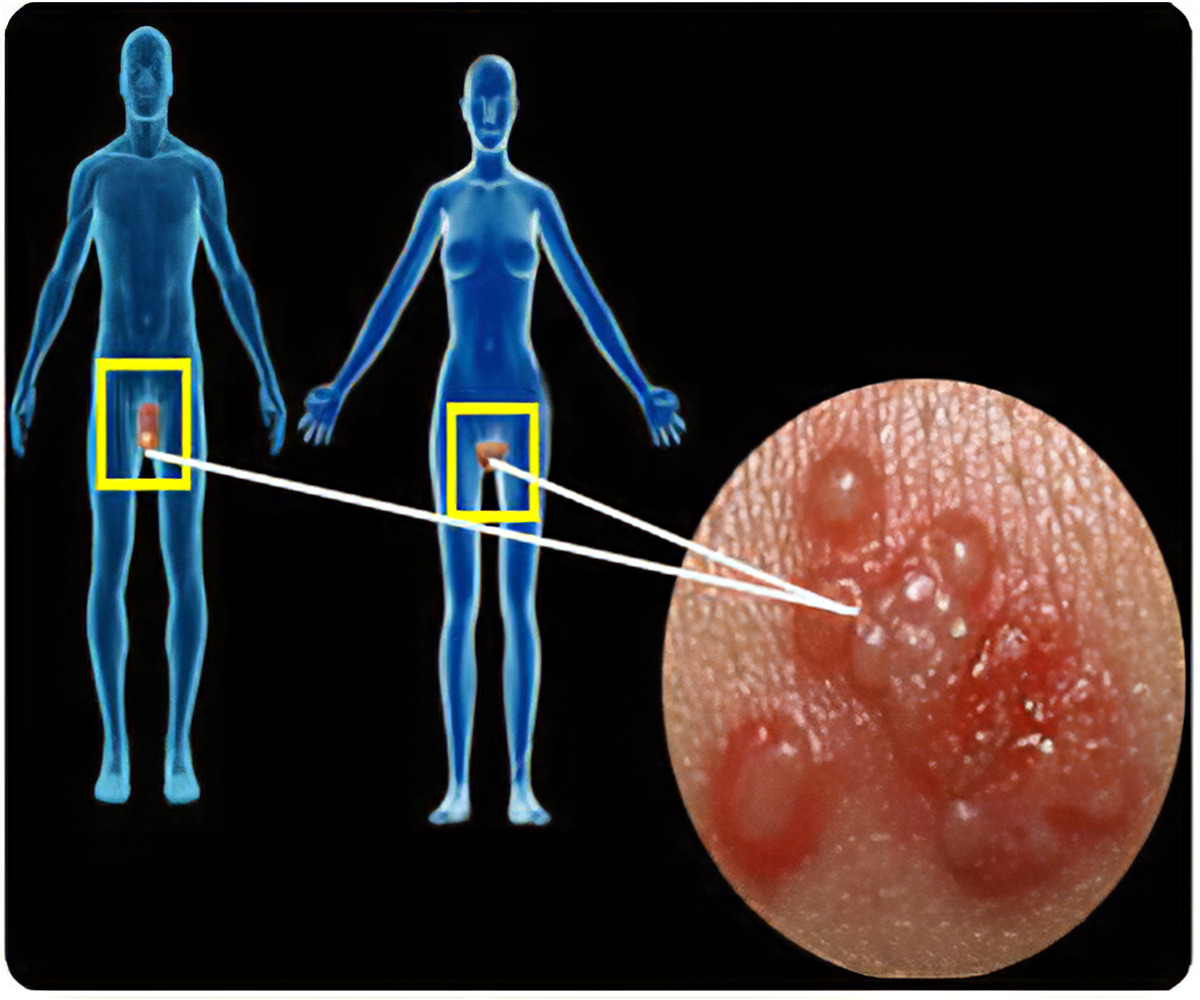
The most noticeable symptom is a lesion or a sore.
They often resemble small pimples or blisters that eventually crust over and finally scab like a small cut. These lesions may take anywhere from two to four weeks to heal fully.
Genital Herpes goes through “dormant” and “active” cycles.
When dormant, the virus retreats to the nerves at the base of your spine. When the virus wakes up and becomes active, it travels nerve paths to the surface of the skin, sometimes causing an outbreak. Depending on the person and whether it’s HSV-1 or HSV-2, the outbreaks can be as many as four to five times a year.
The nerves in the genitals, upper thighs and buttocks are connected; therefore, a person can experience outbreaks in any of these areas.
Such areas include the vagina or vulva, penis, scrotum or testicles, buttocks or anus, or thighs.
A day or two before an outbreak occurs, many people experience an itching, tingling, or painful feeling in the area where their lesions will develop. This is triggered by the virus traveling along the nerve paths and serves as a warning sign.
Genital herpes, regardless of whether it is HSV-1 or HSV-2, does not cause symptoms on the mouth or face.
A person of any age, sex, race, or sexual orientation can get infected with Herpes.
- Having Unprotected Vaginal, Anal, or Oral Sex with someone who has Herpes is the primary way the disease spreads.
Herpes is transmitted via bodily fluids coming into contact with skin. You don’t have to have visible lesions or sores to transmit the disease. Many times, a person who doesn’t know they are infected is responsible for infecting others.
Correct use of a condom will reduce the risk of contacting herpes, but it won’t eliminate it. This is because virus outbreaks can occur on your thighs, buttocks, and other areas not covered by a condom.
The surest way to avoid transmission of genital herpes is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Genital Herpes makes it much easier to become infected with the HIV Virus.
There is an estimated 2- to 4-fold increased risk of acquiring HIV, if individuals with genital herpes infection are genitally exposed to HIV.
This is because the HIV virus needs to enter your bloodstream in order to become active, and the sores from a Herpes Outbreak provide easy access through the barrier of your skin, plus an ideal breeding ground for HIV to replicate itself.
HSV infections can cause major complications for infants born to mothers with the virus. If you are pregnant and have genital herpes, it is even more important for you to go to prenatal care visits. You need to tell your doctor if you have ever had symptoms of, been exposed to, or been diagnosed with genital herpes.
Sometimes, genital herpes infection can lead to miscarriage. It can also make it more likely for you to deliver your baby too early. Herpes infection can be passed from you to your unborn child and cause a potentially deadly infection (neonatal herpes). If you have an active genital herpes infection at delivery, a ‘C-section’ is usually performed.
No. There is no cure for herpes, because any medication strong enough to kill the virus would also damage the nerves at the base of your spine.
However, there are medicines that can prevent or shorten outbreaks. One of these herpes medicines can be taken daily, and makes it less likely that you will pass the infection on to your sex partner(s).
Herpes Test
$149.00Add to cart
A visual exam is not always accurate in diagnosing herpes because the sores associated with the virus resemble several other skin conditions, including, acne, allergic reactions, and even eczema. Many people are misdiagnosed when only a visual exam is performed. A viral culture test can be beneficial in diagnosing herpes. However, an outbreak must be present in order to perform the culture test. The culture is a common method used for identifying the presence of a herpes infection, but it often fails to find the virus even when it is present. HSV infections can best be diagnosed during and between outbreaks by the use of a blood test. The blood test, which detects antibodies to HSV-1 and/or HSV-2 infection, is extremely accurate in detecting the presence of the virus. However, the blood test can not tell you the location of either type 1 and/or type 2 when no symptoms are present.
IgG Test
The Herpes 1&2 Type Specific IgG test is an ELISA test that detects antibodies specific to HSV-1 and/or HSV-2 infection. This test will tell you which type(s) of the herpes virus you have, if either. However, this test does not indicate the site of HSV infection, absent of any symptoms. The IgG test should be taken at least 3 weeks after a contact of concern. It is conclusive at 6 weeks.
IgM Test
The Herpes Types I/II IgM Combination test is also an ELISA test that detects herpes antibodies. The IgM is a non-type specific herpes test and, therefore, cannot distinguish between types 1 and 2. However, IgM levels can provide useful information about a new infection. The IgM may also detect antibodies from a recurring outbreak since those levels may be elevated every time the virus becomes active from its dormant state. The IgM can be taken anywhere between 10 days and 4 weeks after a contact of concern. After 4 weeks, the IgM antibody levels will more than likely not be present.